Depression: Symptoms, Diagnosis, and How an ESA Can Help (2026 Guide)

Let’s get one thing straight. The fog you’re in, the weight you feel—it’s real. This isn’t just a bad mood or a rough patch. You are not alone in this. Statistics show that approximately one in six people will experience a major depressive episode in their lifetime. That’s millions of people who know this fight.
This is a serious medical condition called major depressive disorder, and it requires real attention. But here’s the most important thing I can tell you: it is treatable. There are effective treatments and supports available to help you start feeling better.
Support comes in many forms, from therapy and medicine to the unconditional companionship of an Emotional Support Animal (ESA). An ESA for depression isn’t a cure-all, but it’s a powerful tool for your mental health. Understand how an ESA letter can be helpful for depression treatment.
What Exactly Is Depression?
Depression is a mood disorder. It’s not just feeling sad. It’s a persistent feeling of sadness that hijacks your interest in life, your energy, and your ability to function. It can happen to anyone, including children, adolescents, and older adults.It can feel like a heavy blanket you can’t throw off. This isn’t a character flaw or a sign of weakness. It’s a clinical condition that affects people of all ages, races, and backgrounds.
While it can happen at any age, it often begins in the late teens to mid-20s. It’s a complex illness with different types of depression manifesting in unique ways for each person.
Depression vs. Major Depressive Disorder
According to the American Psychiatric Association (APA), “depression” is a broad term that can describe general feelings of sadness or loss of interest, while Major Depressive Disorder is a clinical diagnosis defined by specific criteria in the Diagnostic and Statistical Manual of Mental Disorders (DSM-5).
In other words, feeling depressed can be part of everyday emotional fluctuations. Still, major depression is a recognized mental health disorder that involves persistent symptoms — such as changes in sleep, appetite, concentration, or self-worth — lasting at least two weeks and causing significant distress or impairment in daily life.
So, while all people with MDD experience depression, not everyone who feels depressed meets the diagnostic threshold for Major Depressive Disorder (APA, 2023).
Common Depression Symptoms
Recognizing the red flags is the first step. If you’re experiencing depression, the symptoms aren’t just in your head. They are physical, too.
Think of this as a checklist. If these points sound painfully familiar, it’s a clear signal to seek help.
Emotional and Psychological Depressive Symptoms
The mental toll is brutal. It’s more than a depressed mood.
- Persistent Sadness or Emptiness: This isn’t temporary. It’s a constant, gnawing feeling that colors everything you do.
- Losing Interest: This is when your favorite hobby feels like a chore. You have no motivation for things that once brought you joy.
- Irritability and Frustration: Small things set you off. You feel constantly on edge, and your patience is gone. This is especially common in men.
- Feelings of Worthlessness or Guilt: You blame yourself for everything. Your low self-esteem is relentless, focusing on past failures.
- Difficulty Concentrating: Your mind feels foggy. Making decisions or remembering details at your job or school becomes nearly impossible.
- Difficult for Building Relationships: Because depression often leads to a desire for isolation, building and maintaining relationships can become a real challenge — whether they’re romantic, friendships, or family connections.
Physical Symptoms
Depression lives in your body. Don’t let anyone tell you otherwise.
Other symptoms are physical and a core part of the disorder.
- Chronic Fatigue: You feel exhausted, no matter how much you sleep. Simple tasks drain all your energy.
- Sleep Problems: This can be insomnia, where you can’t fall or stay asleep, or hypersomnia, where you sleep far too much.
- Appetite and Weight Changes: You might lose your appetite completely and lose weight, or you might crave food and gain weight.
- Unexplained Aches and Pains: Headaches, back pain, and muscle aches without an apparent physical cause are among the most common somatic symptoms. (Source: MedPark Hospital)
Why Does Depression Happen? Causes and Risk Factors
There’s rarely a single cause for depression. It’s a perfect storm of biological, psychological, and environmental factors. Also, hormonal changes may contribute to it, as it happens in perinatal depression.
Your genes also play a part. A family history of depression increases the risk of developing the disorder. So do imbalances in brain chemicals like serotonin and dopamine.
Life can throw things at you that trigger it. Stressful events like trauma, the death of a loved one, or major financial problems can be a starting point. Chronic illnesses like diabetes or heart disease are also significant risk factors. Even hormonal changes, which partly explain why women are more likely to be diagnosed with depression, can play a role.
Depressive Disorder Diagnosis
Getting a depression diagnosis isn’t a scary, mysterious process. It’s a conversation.
A doctor or mental health professional will talk with you about your feelings, thoughts, and symptoms. They will likely conduct a physical exam to rule out other medical issues that can mimic depression.
They use standardized criteria to diagnose depression, like those in the Diagnostic and Statistical Manual of Mental Disorders (DSM-5). This isn’t about slapping a label on you. It’s about unlocking the door to the proper mental disability treatment.
Depression Treatment Options
Here is some real hope: approximately 70% to 90% of people with depression eventually respond well to treatment. You have options.
Think of these as tools for your toolbox. The most effective treatments often involve a combination of approaches.
Psychotherapy (Talk Therapy)
Psychotherapy is about learning to manage your own mind with an expert guide. You build coping behaviors and skills.
Cognitive Behavioral Therapy (CBT) is especially effective. It helps you identify and challenge negative thought patterns that fuel depression. This isn’t just talk; it’s a practical, hands-on way to retrain your brain.
Medications
Let’s discuss depression medicament, also known as antidepressant medication. These drugs help rebalance the neurotransmitters in your brain. They aren’t “happy pills.”
They are a medical tool to correct a biological imbalance. It can take time to find the right one, and you may see some improvement in a week or two, but full benefits often take two to three months. Medications are frequently combined with therapy for the best results.
In cases of severe depression that don’t respond to other treatments, electroconvulsive therapy (ECT) is another highly effective option. (Source: Johns Hopkins Medicine)
Lifestyle Changes and Self-Care
This is the foundation. Professional treatment is key, but self-care strategies support that work.
Regular exercise, a healthy diet, and a consistent sleep schedule are not cures, but they are crucial. Improving these habits is often an important first step in treating depression and managing your symptoms day-to-day.
Does electroconvulsive therapy have evidence in the treatment of depression?
Yes, accordingly to a study published in the Experimental and Therapeutic Medicine periodical, ECT therapy has strong evidence supporting its efficacy in the treatment of depression, particularly persistent depressive disorder that is resistant to medication.
The review of 38 studies and meta-analyses over more than 30 years found that:
- ECT is consistently more effective than antidepressant medications and simulated ECT for achieving symptom remission.
- It produces rapid and significant improvement in severe or medication-resistant depression, including cases with psychotic or suicidal features.
- Safety and tolerability are high, with most side effects (such as transient confusion or short-term memory loss) resolving quickly.
- Continuation therapy with medication or maintenance ECT helps prevent relapse, which tends to occur mainly within the first six months.
- The treatment induces beneficial neurobiological changes, including increased brain volume and enhanced neuroplasticity in cortical and subcortical regions.
The Role of an Emotional Support Animal (ESA) in Depression
Now, let’s talk about a different kind of support. An emotional support animal provides therapeutic benefits to someone with a mental health condition like depression.
Their presence provides companionship, reduces feelings of intense isolation, and offers a reason to get up in the morning. These assistance animals encourage routine and physical activity—taking a dog for a walk can be a huge step on a bad day. The ESA benefits are real and backed by research showing human-animal interaction reduces stress. (Source: UCLA Health)
How an ESA Provides Real Support
It’s about the simple things. Petting a dog or cat releases oxytocin, a hormone that reduces anxiety and increases feelings of trust and bonding.
Caring for an animal provides structure and a sense of purpose. When you feel worthless, knowing that a living creature depends on you is a powerful motivator. They offer unconditional, non-judgmental emotional support, which is priceless when you’re battling your own mind.
Emotional Support Dog vs. Service Animal: Know the Difference
This is a critical distinction. Service animals are specifically trained to perform tasks for a person with a disability and are protected under the Americans with Disabilities Act (ADA). Think of a guide dog for someone who is blind.
Emotional support dogs are not service dogs. They are comfort animals: they provide companionship, but are not trained for specific tasks. Their main legal protection comes from the Fair Housing Act, which helps with housing.
This means ESAs are not allowed in all public places, like restaurants or stores. Under current U.S. regulations, emotional support animals (ESAs) are no longer recognized as service animals for air travel; instead, airlines treat them as standard pets under their pet policies.
Getting Your ESA Letter for Depressive Disorder
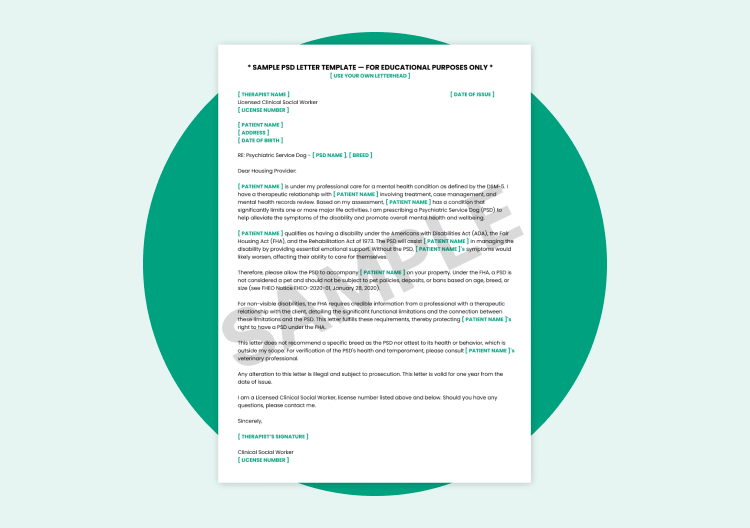
To get the legal protections for an ESA, you can’t just declare your pet one. You need a legitimate ESA letter from a licensed mental health professional (LMHP).
The process is straightforward. You have an evaluation with an LMHP. If they determine that the presence of an emotional support animal helps alleviate the symptoms of your disability, they will issue a letter.
This letter is the documentation you need to request reasonable accommodation from landlords, such as waiving pet fees, under the Fair Housing Act. ESA Pet connects you with licensed professionals to make this process simple and direct.
Get your Official ESA Letter Consultation from a licensed therapist.
Get ESA Letter Now
What to Do If You Have Depression Symptoms
If you are in crisis, do not wait. Your safety is the number one priority.
If you think you may hurt yourself or attempt suicide, call 911 or your local emergency number immediately.
If you need to talk to someone right now, call or text 988 to reach the Suicide & Crisis Lifeline. You can also chat at 988lifeline.org. It’s free, confidential, and available 24/7.
If you feel hesitant to contact a healthcare provider, talk to a trusted friend or loved one. Just telling one person is a brave first step. The most important thing is to get treatment at the earliest sign of a problem.
Taking the First Step Toward Depression Treatment
You’ve read this far, which means you’re ready for a change. Depression can bring significant distress and make everyday life feel overwhelming — but it’s a fight you can win. You don’t have to face it alone.
Take one small, meaningful step today. Talk with your doctor, reach out to the 988 Lifeline, or discover how companion animals can bring comfort, structure, and emotional balance to your recovery. Across many states, people living with post-traumatic stress disorder or other mental disabilities have found that pet ownership offers steady support and relief from isolation.
You deserve to feel better — and to live a life filled with calm, connection, and purpose. Let us help with one piece of the puzzle: get your Emotional Support Animal letter from our licensed mental health professionals and start building the support system you need to move forward.

Emotional Support Animal, Emotional Support Animal Disabilities
ESA Diagnosis: Who Qualifies for Emotion...
Andre Gregatti
Jan 8 2026

Psychiatric Service Dog, ESA and Service Animal Rights, Service Animals
How to Get a Psychiatric Service Dog: St...
Jonalyn Dionio
Dec 23 2025